Learn how physicians are researching melanoma that metastasize to other parts of the body and brain
Melanoma is a specific type of skin cancer derived from melanocytes – cells responsible for skin pigment. Although these tumors can manifest as little moles on the skin, melanomas can be very aggressive and can spread (metastases) to the rest of the body including the brain. Recent advances in immune-based therapy approaches for melanoma have made a significant difference in outcomes for patients with advanced melanoma. While such approaches are quite effective for melanoma metastases in other parts of the body, immune-based therapy approaches are not quite as effective for melanoma brain metastases. A recent study at MD Anderson might have uncovered the reason why melanoma brain metastases are more resistant to treatment than melanoma metastases in other parts of the body.
Michael Davis of the melanoma research at the University of Texas – MD Anderson Cancer Center, and his team examined and targeted mechanisms that melanoma brain metastases exploit to overcome treatment with immune-based strategies.
“Brain metastases are increasingly recognized as one of our biggest challenges in cancer. Melanoma patients with advanced disease have the highest risk of developing brain metastases among common solid tumors, and they are a leading cause of death from this disease…. This research provides new insights into why these tumors may be worse, and it, importantly, found something that might be targetable – oxidative phosphorylation metabolism – with drugs that are in clinical trials now.”
Michael Davis in the Anderson Cancer Center’s report
In order to determine what makes melanoma brain metastases different from systemic metastases, Davis and his team examined genetic changes in both brain and systemic metastatic melanoma tumors from about 74 patients. Their analysis uncovered several novel aspects of brain metastasis. Primarily, they noted the melanoma brain metastases fell into two clusters – long-term and short-term survivors whereby long-term survivors had immune-based signatures. Secondly, they also observed that brain metastases do not allow immune cell penetration when compared to metastases to other parts of the body – hence a huge limitation in treating brain metastases with immune-based approaches. Lastly, the team uncovered and targeted a mechanism that melanoma brain metastases use to resist current immune-based strategies. In essence, these tumors alter their metabolism in the brain in such a way that tumor cells survive despite therapy. Blocking tumor metabolism with a drug currently in clinical trials for other cancers, led to a reversal of tumor persistent. (To read details, please visit the publication, “Molecular Profiling Reveals Unique Immune and Metabolic Features of Melanoma Brain Metastases.”)
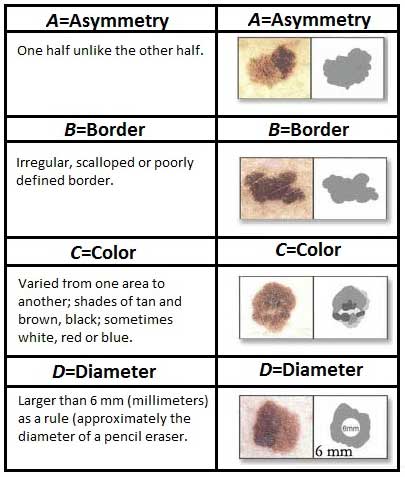
While not thought of as a “bad” cancer, melanoma can potentially move to different parts of the body with the brain being the most worrisome, if not treated properly. Be sure to see your physician if you think you may have melanoma.