The 2018 Nobel Prize in Physiology or Medicine was awarded to scientists who pioneered an innovative approach to cancer treatment that enhances the ability of the immune system to attack and destroy cancer cells – Immunotherapy. Two scientists, James P. Allison and Tasuku Honjo, were awarded “for their discovery of cancer therapy by inhibition of negative immune regulation.” Their discovery centered on unique immune regulatory proteins that serve as immune-checkpoint agents that cancer cells often employ as a way to avoid recognition and destruction by the immune system. Blocking the action of immune-checkpoint proteins with a class of drugs referred to as immune-checkpoint inhibitors results in stimulation of the immune system to engage its cells to attack tumor cells. (You can read details about their findings on the Nobel Prize page.)
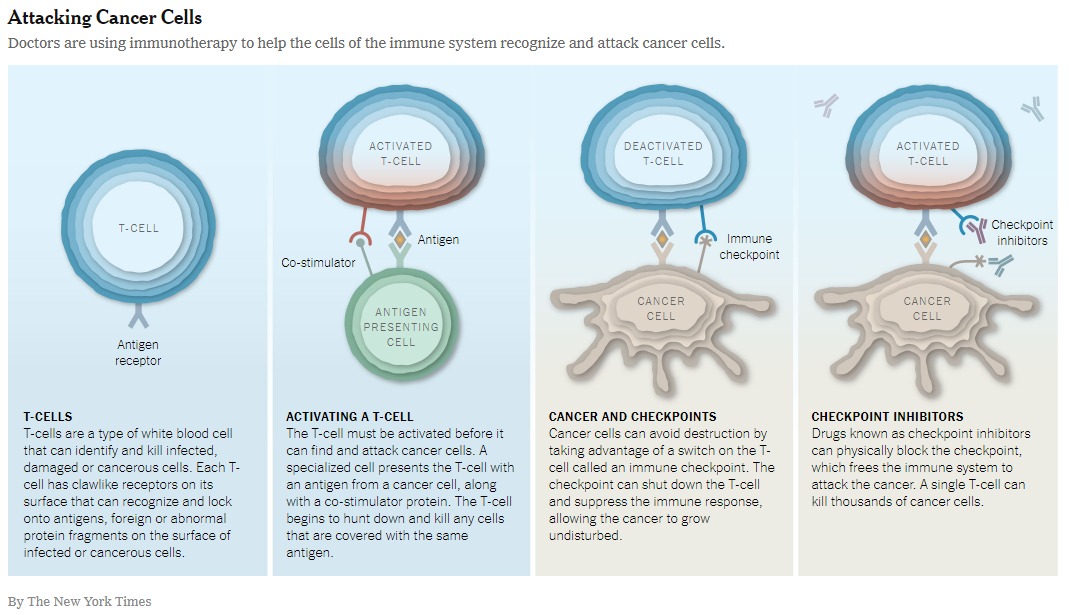
Currently, immune-checkpoint inhibitors have been approved in the United States for Treatment of Cancers such as Melanoma, Lung cancer, Kidney Cancer and others. There are currently trials occurring to determine if immune-checkpoint inhibitors can be effective against Glioblastoma, a very aggressive brain cancer.
The National Cancer Institute (NCI) offers an interesting article, “Can Immunotherapy Succeed in Glioblastoma?” about efforts underway to advance immunotherapy approaches for in brain cancers. Through these efforts, it appears that the immune environment in the brain is not identical to that in the rest of body, hence immune therapies might not necessarily have the same effects in the brain like the rest of body. Furthermore, since our immune systems are unique, there would be a variation in immune response to treatment on an individual basis. Hence identifying the critical patient-related factors (biomarkers) that determine response to immunotherapy is paramount and critical for future success of immunotherapy in brain cancers. Unlike regular chemotherapy, immunotherapy will be more personalized and designed on an individual basis.