Gender is not typically factored into the treatment of cancer, yet it does appear males and females can have distinct gender-specific cancer risks and prognosis. In particular, a recent study demonstrates that there are differences in treatment response to Glioblastoma (GBM) between men and women. The researchers conclude that GBM treatment should be tailored towards known gender-related differences in GBM response to treatment. GBM is a very aggressive and deadly cancer for which there is no cure. While the overwhelming majority of patients die from the disease within 1-2 years, there are a very small number of patients who can live longer due to unique aspects of their tumors. The current standard of care treatment for GBM includes a combination of radiation therapy and the chemotherapy drug called Temozolomide.
The study, published at the beginning of January 2019, is titled “Sex differences in GBM revealed by analysis of patient imaging, transcriptome, and survival data”. It reveals some findings on what is currently used to treat GBM, along with how GBM cancer cells from male and female patients react to treatments.
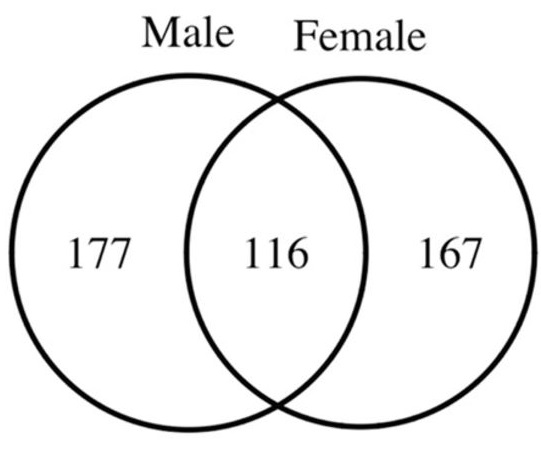
- Chemotherapy sensitivity can be different for men and women. Hence they noted that GBM cells from male patients reacted differently to Temozolomide compared to GBM cells female patients.
- Research includes findings
about the IDH1 mutation difference in women and men. IDH1 mutation confers a relatively good prognosis compared to tumors without IDH1 mutation. - They further showed the GBM survival was different between males and females.
- Lastly, the researchers were able to identify unique genetic clusters that correlated with a sensitivity to chemotherapy
Overall, they suggest that physicians may employ gender or sex-based difference in cancer treatment response in the future to treat patients in the most effective manner. As they state, “These studies emphasize that analyses without consideration of sex can obscure critical elements of biology and, in aggregate, highlight the importance of parallel but separate analyses of male and female cells, male and female animals, and male and female patients.”
Dr. Etame shares: “Basically, it seems women have a better outcome with GBM treatment compared to men. It also looks like there are distinct biological pathways that promote tumor growth in each of the sexes. Identification and further characterization of such pathways could in the future allow for personalized treatment strategies.”
Further highlighting the role of gender in cancer risks is another study that was published in 2017. Since males have only one X-chromosome while females have two X-chromosomes, the researchers were determined that the presence of only a single X-chromosome in males increases the risks of cancer in men compared to females. Read more on their publication, “Tumor-suppressor genes that escape from X-inactivation contribute to cancer sex bias.”
As more research emphasis is placed on the gender-related differences in cancer risks and prognosis, it is anticipated that these research advances will be translated clinically in the management of patients with cancer as part of a personalized cancer care paradigm.

